Every fertility center in the United States is required by law to report their IVF Success Rates to The Centers for Disease Control and Prevention (CDC). The CDC takes three years to collect the data for each year’s cycles. This is because the outcome of pregnancies is not immediately known. Additionally, analyzing data and preparing it in a uniform reporting style takes time. While the CDC report contains the current national data, SART provides reports within two years for their member clinics.
Who is SART?
The Society for Assisted Reproductive Technology (SART) reports on success rates for most fertility clinics in the nation. The SART charts also include information about annual fertility clinic activity and success, including the ages and types of clinic patients. SART reports the most recent IVF success rates for their member fertility clinics. Not every fertility clinic in the United States is a member of SART. For 2010, SART had 370 clinics reporting, while the CDC has a total of 443 reporting. www.sart.org
Infertility Guide to Understanding the IVF Success Rate Report:
The statistics provided by SART and the CDC can tell you a lot about a practice, but if you’re not a statistical reader or numbers geek it may be difficult to filter out the relevant information to make a decision. Here are a few helpful tips on what to look for and what it may mean to you.
3 Most Important Things to Note:
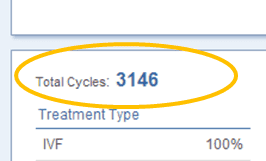
1) The number of cycles a clinic performs.
2) The percentage of cycles resulting in live births.
3) The average number of embryos transferred.
- Data is not the same across the board. Although the CDC guidelines instruct clinics on how to report their cycles, there are individual variables that impact success rates. Clinics that complete greater numbers of IVF cycles will show less variation year to year than clinics that complete fewer cycles.
- Some clinics accept “more difficult” cases into their program where other programs have age and diagnosis cut offs. Our fertility declines with age and patients with ovarian reserve issues can be poor responders during an IVF cycle. Some clinics will not accept these patients into their program without using donor eggs. That patient’s potentially failed cycles will lower the clinic’s success rates.
- Success rates are reported per cycle, instead of per patient. Patients who cycled several times and failed before finally conceiving may lower a clinic’s success rates because each of her cycles counts as individual failures and only one success.
- Cancellation rates vary. Some clinics cancel more cycles than others. That leads to a lower percentage of live births, but may increase the number of retrievals resulting in live births and the number of transfers resulting in live births. In short, depending on how strict a clinic is with their cancellation guidelines, their success rates can change.
- Natural cycles (without medication) and medicated cycles are included in the same data. Natural cycles typically produce fewer eggs for retrieval, thus fewer embryos to become live births.
- Number of embryos transferred varies from clinic to clinic. Some clinics opt for double embryo transfers (or more in those over the age of 35), while other clinics encourage Single Embryo Transfer (SET). Transferring more embryos does not increase your odds of getting pregnant, but it does increase the risks associated with a multiples pregnancy, can result in pregnancy loss, or lead to premature birth.
Of course then you factor in things like egg quality, sperm quality, the skill of the doctors, the use of advanced equipment, the health of the patient, and potential problems on a chromosomal level. All of these things can impact a fertility clinic’s success rates. So, when it comes to looking at fertility clinic IVF success rates, make sure you understand what you’re really looking at.