Polycystic ovary syndrome is a common hormone disorder that affects 5-10% of all women in their reproductive years. PCOS accounts for nearly one-third of all infertility diagnoses and is very common among women with ovulatory disorders.
PCOS is one of the most underdiagnosed diseases in the United States, and surprisingly, most women who have it do not even know it.
The truth is that most women are never officially diagnosed with PCOS until they start attempting to get pregnant. Difficulties with getting pregnant may be due to the irregular cycles that accompany PCOS and may require some type of treatment to improve the chances of pregnancy.
In an effort to shine a brighter light on this condition today, PCOS Advocacy Day, RMA Networks Dr. Leo Doherty is lifting the fog on polycystic ovarian syndrome.
What is Polycystic Ovary Syndrome?
Polycystic ovary syndrome is a hormonal imbalance disorder that affects up to 20% of reproductive-age women. Because the condition affects the body’s hormonal processes, it has an effect on ovulation and fertility. Many women with PCOS will have trouble conceiving naturally, but with the right treatment, chances of pregnancy are good.
Reproductive hormones are abnormally regulated in women with polycystic ovarian syndrome. The usual interplay between hormones that results in the maturation of eggs and ovulation is abnormal, causing:
- Infertility (due to irregular/absent ovulation)
- Irregular periods
- Elevated androgen levels (Testosterone) can cause symptoms such as acne and unwanted hair growth on the face and other parts of the body.
Lack of ovulation over time can lead to abnormalities in the uterus, where the endometrial tissue can become thickened. This leads to heavy or irregular periods and, in extreme cases, endometrial cancer. Many women with polycystic ovary syndrome also demonstrate insulin resistance, which makes them prone to weight gain and diabetes.
The number of eggs within a woman’s ovaries is finite and gradually reduces over time. From puberty to menopause, women will go through hundreds of thousands of eggs. During that time, only a small percentage of these eggs ever ovulate. In a perfect world, the hypothalamus, pituitary gland, and ovaries all work together each month to grow follicles and release an egg.
OK, let’s break that down…
A runner’s analogy, if you will:
- Each month, a number of eggs are present in follicles and can be stimulated for maturation and ovulation. We’ll call these follicles runners.
- In a normal menstrual cycle, the hypothalamus, pituitary, and ovary interact to stimulate one follicle (and the egg inside) to grow and mature.
- That follicle (runner) will reach ovulation (the finish line). The runners that didn’t get stimulated are degraded in a process known as atresia.
- Next month, there is a whole new group of runners, and these monthly “races” will continue until menopause.
- In women with PCOS, there are many more runners than usual in the monthly race for ovulation, but they never reach the finish line (ovulate), so there is no winner.
- In other words, there are a lot of follicles, but they are not maturing properly and not releasing an egg. As women get older, the number of runners decreases, and so do their chances of pregnancy.
Why do some women get polycystic ovarian syndrome and others don’t?
We know genetics play a large role in who develops polycystic ovary syndrome. First-degree relatives of women with PCOS (mothers and sisters) have up to a 30-50% chance of developing the condition.
There are also other theories about the cause of PCOS, such as the effect of the in-utero environment on the risk of developing PCOS later in life. In-utero exposure to elevated levels of testosterone, fetal undernutrition, and elevated AMH levels have been implicated in the development of PCOS.
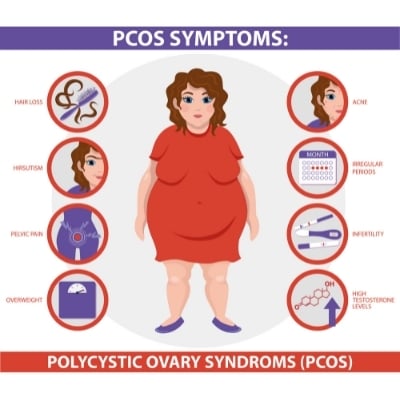
What are the symptoms of polycystic ovary syndrome?
The most common symptoms of PCOS are:
- Irregular periods or a loss of menstruation entirely
- Acne and abnormal hair growth (commonly on the face, chest, or abdomen) are commonly seen due to elevated androgen levels
- Obesity, difficulty losing or maintaining weight, and type 2 diabetes are also common
- Infertility can be a presenting symptom in couples trying to conceive
- Anxiety, depression, and eating disorders are also seen in patients with PCOS
How is PCOS diagnosed?
It’s important to note that not all women who have menstrual irregularity have PCOS. In order to be diagnosed properly, there are three specific qualifying criteria that a woman must meet:
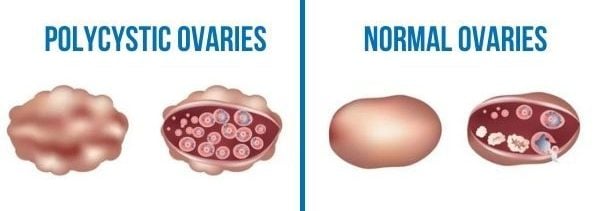
- Multiple small, immature follicles on the ovaries, as seen on an ultrasound
- Irregular menstrual cycles
- Elevated levels of androgens (male hormones) in blood or clinical evidence of increased androgens (mostly increased hair growth).
The diagnosis process:
The physician will record the patient’s medical history when beginning the diagnostic process. They will note how often the patient menstruates and will calculate their body mass index (BMI).
The doctor will also perform a transvaginal ultrasound to check for multiple immature follicles on the ovaries.
If indicated, an endometrial biopsy may be performed – where a sample of a woman’s endometrial tissue is examined – can screen for endometrial hyperplasia or cancer in women who have had prolonged amenorrhea (lack of a period).
A series of bloodwork will help the doctor make the final diagnosis, specifically looking at certain hormone levels:
- FSH (Follicle Stimulating Hormone)
- LH (Luteinizing Hormone)
- AMH (Anti Mullerian Hormone)
All of these hormones play an important role in ovulation. These levels can help a doctor understand the state of a woman’s fertility.
The most important of these hormones for a diagnosis is AMH. AMH is a hormone secreted from a woman’s follicles as they mature.
Because women with PCOS have many more follicles that are maturing (albeit improperly) than a woman without PCOS, their AMH count will be higher than normal and alert doctors to the woman’s condition.
For example, an AMH level below 3ng/m is seen as healthy during a normal cycle; an elevated AMH level of 4 ng/m or higher can be a marker of PCOS.
Once a doctor makes a PCOS diagnosis, treatment is available for patients trying to conceive.
How is PCOS treated in women who want to conceive?
The first line of treatment for women with PCOS is lifestyle modification. Dr. Jackie Gutmann explains how you can learn natural ways to boost your fertility here.
Modest weight loss and increase in lean muscle mass can have huge impacts on abnormal hormone regulation.
In order to conceive, medications are often needed. The goal of treatment is to correct ovulation.
Ovulation Inducing Medications
A woman may be prescribed Clomid, an ovulation-inducing medication that indirectly promotes the production of FSH and the growth and release of a mature egg. Another medication commonly used to induce ovulation in women is Letrozole.
Intrauterine Insemination (IUI)
After ovulation is induced with Clomid or Letrozole, the doctor may recommend timed intercourse or intrauterine insemination (IUI). Injectable FSH with IUI can also be used in women with PCOS.
In Vitro Fertilization (IVF)
In vitro fertilization (IVF) is another excellent treatment for women with PCOS and has superior success rates and a far lower chance of a twin or triplet pregnancy.
Options for women not trying to conceive
The first treatment for women not trying to conceive is behavioral change, such as weight loss, healthy eating, and exercise. Birth control pills and insulin-sensitizing medication (Metformin) can also be given to improve irregular periods.
Are there other risks to women with polycystic ovarian syndrome?
- Metabolic syndrome is common in patients with polycystic ovary syndrome.
- There is also a higher risk of heart disease.
- Patients are also at risk of developing overt hypertension and diabetes.
- Another risk factor is endometrial cancer. Because women with PCOS often don’t have regular menstrual cycles, they have higher levels of estrogen. Higher levels may cause a thickening of the uterine lining. Pre-cancerous and cancerous cells may develop when the uterine lining is thicker than normal.
- Depression is also more common in women with polycystic ovarian syndrome. It is important for patients to identify any changes in their mood so that they can seek appropriate treatment.
Is there a cure for polycystic ovary syndrome?
For those women who have developed PCOS on the basis of excess weight, the diagnosis can be reversed. Maintaining a healthy weight and overall healthy lifestyle is the most productive way to offset symptoms.
In the cases where genetics play a role, there is no cure, but treating the symptoms can result in pregnancy.
For women past their childbearing years, it is still important to seek treatment for PCOS. The lack of ovulation can result in a buildup of the uterine lining, leading to periodic heavy menstruation and, in rare cases, uterine cancer.





