It is best to seek the assistance of a fertility specialist if you are younger than 35 and haven’t been successful in achieving a pregnancy in 12 months. It is recommended for couples older than 35 after trying for 6 months.
We know that coming into a fertility clinic for testing can be stressful when you don’t know what to expect. To help, our fertility specialists have put together a blog outlining everything you need to know. We’ll introduce you to the different types of infertility tests and prepare you with a general idea of what constitutes a positive or negative result for each test.
Types of Fertility Tests for Women
When you visit an RMA fertility clinic, our specialist will want to talk to you about your full medical history and any previous treatments you may have had, including a review of the results from any previous infertility tests.
He or she will also probably want to perform a general physical examination of both partners where appropriate to assess your general health. Not all types of infertility tests will be needed for each case, so this baseline assessment can give the specialist an idea of where to start.
Infertility tests fall into two main types:
- Blood Tests: First, there are blood tests that can analyze the presence and/or quantity of different hormones.
- Imaging: The second type is imaging, which can help the fertility specialist ‘see’ inside your reproductive system to identify the problem.
Fertility Blood Tests
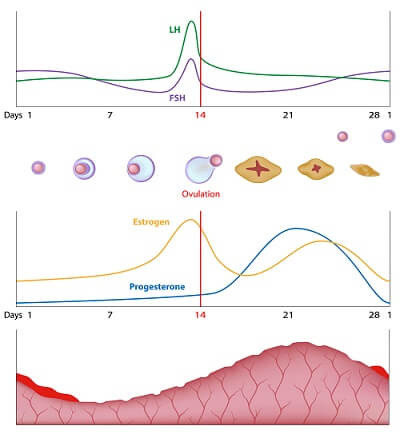
The human body naturally produces a range of powerful hormones, each of which plays a different role in the complex system that regulates menstruation, ovulation, and the reproductive cycle, including pregnancy. Too much or too little of one can impact the others and upset this delicate balance. Bloodwork helps a physician assess these hormones. Usually, your doctor will order them before any fertility treatment can be started. Sometimes a test previously carried out within the last 6 – 12 months can be used, but a fresh test is often required.
When considering the results of the various hormone levels, it is essential to remember that they vary between individuals and can indicate different things according to many factors, such as age and general health history.
Estradiol
Estradiol is one of the most potent of the group of steroid hormones known as estrogens. It controls the development and maintenance of female sex characteristics and acts on female reproductive organs, including the lining of the vagina and fallopian tubes. Estradiol is produced by the growth of follicles, the tiny sacs containing eggs in the ovaries, and results in the production of fertile mucous from the cervix, as well as prepares the lining of the uterus for a fertilized egg, or embryo, to implant.
- Estradiol levels are measured in picograms per milliliter (pg/ml).
- Normal levels vary widely depending on your menstrual cycle phase, ranging between 30 to 400 pg/ml.
Anti-Müllerian Hormone (AMH)
Anti-Müllerian hormone is produced primarily in a woman’s ovaries.
- AMH blood levels are measured in nanograms per milliliter (ng/ml).
- Normal levels are considered at least over 1.0 ng/ml, although very high levels may indicate another problem.
Follicle Stimulating Hormone (FSH)
Follicle-stimulating hormone is produced by the pituitary gland in the brain. Its levels in the blood fluctuate according to the menstrual cycle. A rise in FSH during the first half of the cycle stimulates the growth of the egg-containing follicles, and as they mature, it acts together with other hormones to trigger ovulation. After ovulation, feedback to the pituitary inhibits the release of FSH, making levels lower.
- FSH is measured in milli-international units per milliliter (mIU/ml).
- A good level for a baseline test, when FSH should be low, is probably less than 10 mIU/ml. Still, results need careful interpretation by a fertility expert as part of the overall hormone balance.
- Abnormally high FSH levels can be an indicator of a low ovarian reserve.
Luteinizing Hormone (LH)
After initial stimulation of the follicles by FSH during the first part of the menstrual cycle, a surge in LH produced by the pituitary gland stimulates the release of an egg from the follicle, or the process known as ovulation. A measurement of this surge is often used to predict a woman’s most fertile period.
Progesterone
Progesterone prepares the lining of the uterus by stabilizing it to be ready for the implantation of a fertilized egg, or embryo, following ovulation. If you become pregnant following ovulation, progesterone levels increase and help sustain the pregnancy. If you do not become pregnant, levels of progesterone decline, which helps trigger the onset of a menstrual cycle.
- In a regular menstrual cycle, progesterone levels fluctuate throughout the month.
- You would expect the highest levels in the middle of the luteal phase of your cycle, and usually, concentrations of more than 3 ng/ml suggest that you have ovulated.
- Levels of 8-10 10 ng/ml are desired for pregnancy.
Androgens
It is usual for small amounts of the ‘male hormones” or androgens, such as testosterone and DHEA-S, to be produced in women. However, excess production leading to abnormally high levels could interfere with developing ovarian follicles and ovulation. Elevated testosterone levels are often found in polycystic ovary syndrome (PCOS), which can be associated with infertility.
- Testosterone in the blood is measured in nanograms per deciliter (ng/dL).
- Normal levels in women are between 15 and 70 ng/dL.
- Levels that are either lower or higher than this range can cause problems with fertility and other symptoms.
Prolactin
Prolactin has many functions, but it is most commonly known to stimulate milk production in those who are breastfeeding. It is also elevated in pregnancy. Without pregnancy, the body typically has low levels of this hormone. High levels could be a side effect of some medications or be produced by slight growth in the brain’s pituitary gland, which can result in menstrual irregularities.
- An average level of prolactin for non-pregnant or breastfeeding women in most labs is less than 25 ng/ml.
- Almost all cases of hyperprolactinemia are easily treated with oral medications.
Thyroid Hormones
An underactive thyroid is known as hypothyroidism. Recent research by a team from Harvard Medical School has shown that low thyroid function among women with unexplained infertility was twice as common as among women without the condition.
Blood tests for thyroid levels typically measure the amount of thyroid-stimulating hormone (TSH) from the pituitary. With low circulating thyroid hormone levels, the brain works overtime to restore the optimum level.
- TSH is measured in milli-international units per liter (mIU/L).
- A normal level of TSH is in the range of 0.4 to 4.0 mIU/L, with levels above this range usually indicating an underactive thyroid.
It’s important to remember that with all these blood tests, a single measure of a particular hormone cannot be considered diagnostic of fertility or infertility, as hormones constantly fluctuate. For some hormones, the day the measurement is taken in the menstrual cycle is critical; in others, there may be reasons for abnormal results unrelated to fertility. A skilled and experienced fertility specialist is essential to interpret blood test results and make treatment recommendations.
Imaging tests for infertility
Some fertility tests allow the physician to form a picture of the inside of the reproductive system and are essential in reaching a diagnosis. Ultrasound, hysterosalpingogram, and saline sonogram are examples of such tests and may be needed depending on your case.
Ultrasound scan: what is it?
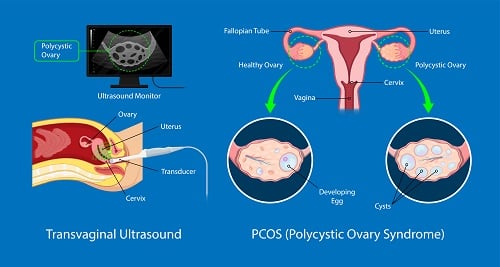
The ultrasound technique uses high-frequency sound waves to create a real-time picture of the internal organs on a monitor.
It can monitor ovulation, detect early pregnancy, and check for pelvic masses or other problems. It is also commonly used in fertility treatment for monitoring a patient’s response to follicle-stimulating hormones and in IVF treatment, where ultrasound is used to guide the retrieval of oocytes or eggs.
Hysterosalpingogram (HSG): what is it?
The hysterosalpingogram test is a 15-minute office procedure. It can show uterine abnormalities such as polyps and fibroids or reveal scar tissue blocking the fallopian tubes.
FAQ
What happens during an ultrasound?
- During the test, the patient lies on an adjustable table with her feet in stirrups.
- X-ray is positioned above the pelvis.
- The physician places a speculum in the vagina, like when you have a pap smear, and inserts a small catheter, or tiny tube, through the natural opening of the cervix.
- Contrast is a liquid that will be passed through the catheter into the uterus and flows into the fallopian tubes.
- The real-time X-ray image produced by fluoroscopy will be displayed on a screen so the physician can see the outline of the uterus and tubes and determine whether there is any evidence of blockage preventing the flow of liquid.
- This test may produce slight cramping when a blockage is present, but the test may cause no discomfort when expected.
What do the results mean?
Having seen the shape of the inside of the uterus and determined the patency of the fallopian tubes, the physician will be able to discuss the results immediately with the patient and make recommendations for how to proceed with fertility treatment.
Saline Sonogram: what is it?
A saline sonogram, also known as a sonohysterogram, is also a 15-minute office procedure. It is similar to the hysterosalpingogram in that it allows the physician to see an image of the inside of the uterus. In this case, the image is produced by ultrasound.
How accurate are infertility tests?
No single test can give a definitive diagnosis of infertility or its reasons. However, when our fertility specialists at RMA have completed all the necessary testing and evaluations, they will have all the information they need for an accurate diagnosis and an optimal treatment plan.
Blood tests measuring FSH, AMH, and estrogen levels will provide important conclusions about egg quality and quantity. At the same time, a transvaginal ultrasound can assess follicle count and identify any structural abnormalities. A hysterosalpingogram will determine whether your fallopian tubes are functioning normally or are blocked, and a saline sonogram gives more information about your uterine cavity.
Combined, with the benefit of the fertility specialist’s accumulated knowledge and experience, these tests will provide an accurate assessment of your diagnosis and aid in treatment planning.
How much do infertility tests cost?
Rates for infertility testing vary according to the type of test and from clinic to clinic, so it is impossible to give a list of applicable prices. The Society for Assisted Reproductive Technology (SART) explains that costs for fertility treatment vary according to the treatment center, patient profile in that center, and insurance coverage.
The most significant factor of these is insurance coverage. For example, a popular price checker site estimates between zero and $30 or more for blood tests for patients with insurance or from $700 to $2,589 without.
Our financial counselors at RMA can help to answer queries about cost and insurance coverage and guide you through the complexities of the financial process.
Here are some key points to consider about funding fertility tests and any subsequent fertility treatment:
Understanding the cost breakdown
An online search for the cost of fertility treatment will return a lot of information about IVF, the best-known and most successful fertility treatment. Still, it can be hard to separate what your initial investment will be if you only want to clarify the costs associated with the infertility testing stage.
Some clinics offer an à la carte-style service, each process identified in the cost breakdown. For example, the first four steps of any fertility treatment are likely to be:
Cost vs. value
If you intend to go ahead with fertility treatment and your test results show it is needed, you must think hard about the cost/value ratio when choosing your clinic.
For example, it may be more expensive if your fertility center has a state-of-the-art embryology lab, an outstanding medical team, and excellent success rates. But in terms of value in achieving one healthy baby in as few cycles as possible, along with the lowest possible risk to both mother and child, it could work out much better.
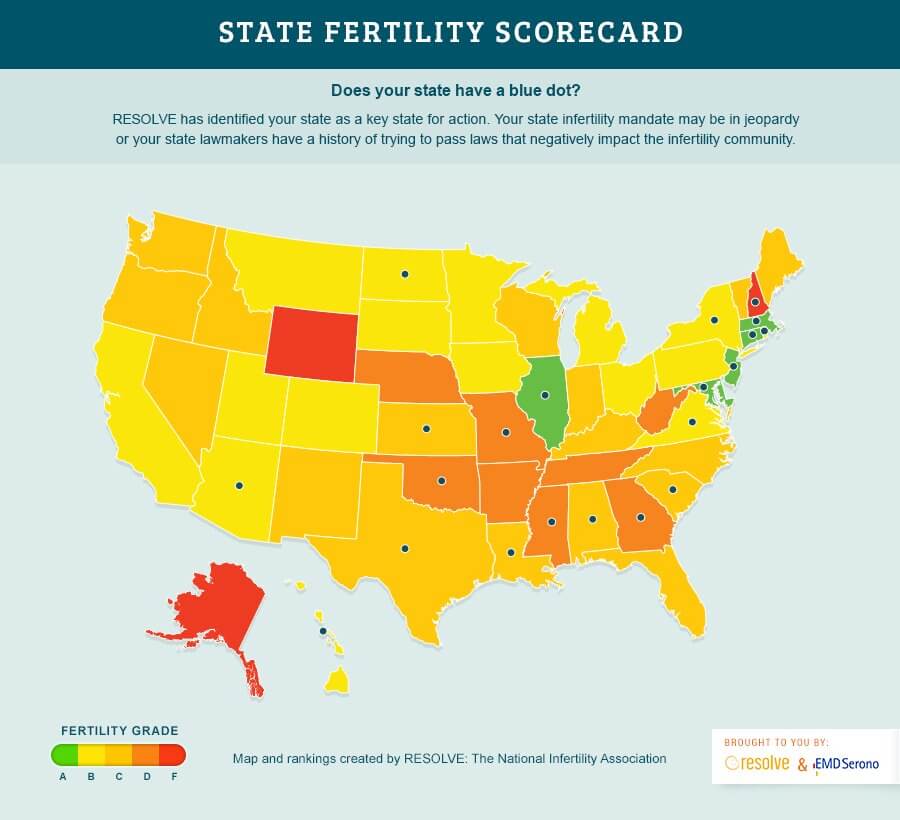
Fertility insurance coverage
The good news about the cost of infertility tests is that the prices you get from a prospective clinic will not necessarily reflect your actual cost. Everything will come down to your insurance coverage. We at RMA strongly recommend that you talk to your insurance carrier and get clarity on the exact extent of your coverage. Here are a few points you need to cover concerning infertility testing:
- What are the exact details of your coverage?
- What diagnostic tests are included?
- Are any diagnostic tests excluded?
- Is ultrasound imaging covered?
- Are any medical criteria to be met before approval for testing or treatment?
Look at our article on the cost of fertility treatment for more specific pricing information. There’s a lot of helpful information on the RESOLVE state fertility scorecard, options for fertility financing, and tips on evaluating your intended clinic’s cost/quality ratio.
If you’re still looking for more information on fertility testing, we recently compared at-home fertility tests to the testing we perform in-office.
Contacting RMA
We at RMA strive to make the path to parenthood ever safer and more successful. We do this through our investment in research, resources, staff, and advanced technologies that lead the way in reproductive medicine.
Living, joyful evidence of our success is the 40,000 babies born to loving families across the US and abroad. If you’d like to find out more and discuss your fertility options with us, just get in touch through our online contact form.